Engagement means creating the right conditions for all the individuals involved in improvement to be motivated and able to contribute to the best of their ability. This means people both inside and outside your organisation, though you are likely to have more influence internally.
The more engagement you generate, the more successful and sustainable your improvements will be. Get the engagement right, and your team will participate, leaving you time to be more strategic. They are also likely to learn improvement skills they can then use when they spot other issues that need sorting.
Download RCGP Quick guide: Engagement and Behaviorial Change
The first step is to think carefully about who are the people you need to ‘engage’ with. These are your ‘stakeholders’ and they include everyone that will feel an impact from your project, either because they will be involved in implementing or testing out changes, or they may feel the impact of the change itself.
Engagement has a different purpose according to what role the stakeholder plays in the project. A communication strategy is described in another QI guide that can help you to work out what level of communication to have with each type of stakeholder. Involving your patients in designing and monitoring improvements can be an excellent way of engaging them and reducing resistance to change.
Getting engagement (or ‘buy in’) from the GPs and practice staff can be challenging especially when day-to-day workload is high and it is best achieved:
- Running effective meetings using tools to maximise participation
- Using an understanding of the strengths and personalities in your team
- Understanding of human motivation theories and how to apply them
How to
1. Running Effective Meetings
- QI meetings often have a different ‘feel’ to them than business meetings. Though it is very important they are facilitated, and action points recorded, it is often useful to allow more time for creative ideas to develop.
- Many of the tools described in our Quick Guides (e.g. SWOT analysis, Fishbone diagrams, Context checklist, Process-mapping and the Model for Improvement) can be used during QI meetings to achieve a shared understanding of the issues for improving and to plan action.
- Participants in meetings often find it easier to contribute of they work in pairs first, before sharing their thoughts with the whole group. This can work well when you are exploring the root causes for a difficult issue prior to constructing a Fishbone diagram.
- Writing ideas on post it notes and then collating them on the wall encourages participation from the quieter members of a group.
- Try not to achieve too much in each session and at the end of the session summarise where you are up to with the ‘Diagnosis’ of the issue and what the next steps might be. Clearly allocate the actions points with a realistic deadline and then arrange the next meeting date.
2. An understanding of the strengths and personalities in your team
- Your team will perform best when they are playing to their strengths. The Belbin Inventory of Team Roles is used to score people on how strongly they express the behavioural traits from nine different team roles. It is widely used and is a useful tool for gaining a better understanding of the strengths of your team and building on them.
- This will both help all to engage appropriately with your QI work and also gain a better understanding of how to work with each other.
3. An understanding of human motivation theories and how to apply them
- Effective quality improvement usually requires us to start to behave differently. Often this is by starting to respond differently to comments from patients, or to start to value measurements and data. It usually involves us accepting that things might be better done in a different way and human beings seem to generally feel uncomfortable with change. We need to understand how to motivate others to maximize engagement.
- People are motivated by an array of factors. For some, improving the quality of care to their patients is enough, particularly if not taking action will have dire consequences for their patients. For these people gathering and displaying data showing how things are improving, and sharing and celebrating positive feedback from patients will be very motivating.
- For others, professionalism or subject matter being of interest or alignment with personal or organizational goals might be key, and they may be more motivated by external recognition, for example by GP peers or the CCG/cluster.
- Other possible levers are the threat of coercion, poor inspection outcome or incentives (a gain in time, money or other resources). GP contracts over recent years have often been aligned to payment for performance, and though these techniques have been shown to lead to better performance in the individual items measured, they have not led to better outcomes for patients.
- It is thought by some that financial reward for achieving an externally imposed target may actually demotivate many people and distract them from aiming for better overall care for patients.
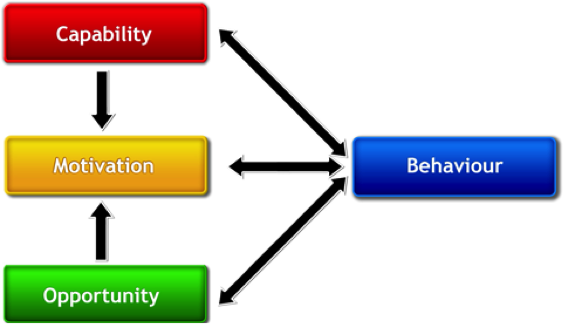
Michie et al have developed a framework for understanding behaviour. In their framework, capability, opportunity and motivation interact to create behaviour.[1]
Capability is defined to include having the knowledge and skills to engage. Opportunity refers to external factors that can influence the adoption of the intervention. Motivation is creating the energy that will direct behaviour.
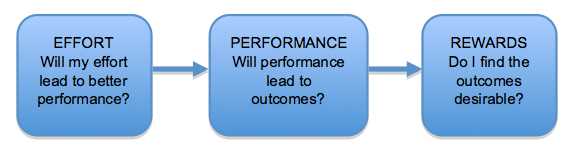
Vroom’s Expectancy theory describes how peoples’ motivation to perform is influenced by 3 factors:
- Whether they believe in the benefit of the desired outcome. (Valence)
If you are leading an improvement project it is helpful if you have a clear idea of the benefit yourself. If you know of where, for example, encouraging on line booking has reduced practice workload, then share the story to motivate others. If you can show the harm that can be caused by the overprescribing of antibiotics, then this will increase motivation.
- Whether they believe the effort they are putting in to the project will actually result in better performance (Expectancy)
If they can see the whole team is pulling together and that the project is being prioritised by the practice, this encourages positive expectation. Motivation will also be lifted by you confidence, as leader, in the methods you are using to bring about change.
- Whether they believe that good performance will result in achieving the desired outcome (Instrumentality).
As the leader of the project, giving examples of where change has taken place elsewhere using similar methods can help to motivate others. Individual motivation will also be increased by gathering data during the project showing you are moving towards your aim. This can promoted further by identifying quick wins and celebrating them.
MOTIVATION = EXPECTANCY x INSTRUMENTALITY x VALENCE
[1] Michie S, et al. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science 2011; 6:42; DOI: 10.1186/1748-5908-6-42.


